The issue of polypharmacy among children, particularly the use of multiple psychiatric drugs, has become a pressing concern in the realm of mental health treatment. Joe Hoft discusses the alarming rise in this practice, illustrated by a study led by Dr. Lawrence Kleinman from Rutgers. The research analyzed Medicaid data for over 141,000 patients under the age of 21 who were prescribed psychiatric medications, revealing that a significant number—nearly 400—were given potentially unsafe combinations. Kleinman emphasizes the need for informed consent, asserting that patients and their caregivers should be made aware of the risks associated with these drug cocktails, which are often prescribed in contravention of established medical guidelines.
Within Kleinman’s research, the findings indicate that polypharmacy is not a rare occurrence; about 38 percent of the patients received multiple psychiatric medications simultaneously. The study identified the antipsychotic Ziprasidone among the most commonly contraindicated drugs, often paired with antidepressants like Fluoxetine (Prozac) and Trazodone. Kleinman’s findings echo earlier reports from Maryland that indicated a rising trend of children receiving overlapping psychiatric drugs over extended periods, raising ethical questions about the prescribing practices and the implications for vulnerable populations like those in foster care. These revelations highlight a troubling trend where dangerous polypharmacy is being normalized in pediatric care despite known risks.
Further complicating the issue is the significant uncertainty surrounding psychiatric diagnoses and the efficacy of the medications prescribed to treat them. A separate article on Axios delves into the ongoing challenges doctors face regarding the treatment of complex mental health conditions, revealing that prescribing psychiatric drugs often entails a trial-and-error approach, frequently leaving patients exposed to unnecessary side effects. The authors point out the lack of concrete scientific evidence to substantiate the existence of psychiatric disorders or their treatments, leading to skepticism over the rationale behind prescribing multiple medications.
Adding to the complexity, Hoft argues that no definitive tests currently exist to assess the conditions purportedly treated by psychiatric medications, undermining the validity of their effectiveness. Instead of being based on objective medical data, many psychiatric diagnoses rest upon subjective evaluations and assumptions. For instance, the “chemical imbalance” theory—the notion that psychiatric disorders stem from neurotransmitter deficiencies—has been thoroughly discredited, illustrating a substantial gap in understanding how psychiatric drugs, such as Prozac and Zyprexa, actually work. In fact, the FDA explicitly states that the mechanisms underlying many psychiatric medications remain largely unknown, thus raising eyebrows about their safety and appropriateness, especially in children.
The potential dangers associated with these psychiatric drugs are alarming, as adverse effects—including anxiety, psychotic episodes, and even suicidal thoughts—are documented for many commonly prescribed medications. When considering a scenario where multiple drugs could be prescribed to a child, the question of informed consent becomes paramount. Are patients and their families fully educated regarding the risks of the drug combinations prescribed to them, especially given that there is no clear scientific backing for these treatments?
No regulatory body oversees the prescriptions and administration of these psychiatric drugs to children, with significant implications for patient safety. The absence of guidance on the number of medications a child can be prescribed creates an environment conducive to mismanagement and hazardous health outcomes. Furthermore, a lack of information shared with patients regarding the process for reporting adverse effects exacerbates the challenge. Amidst these systemic failures, the glaring reality is that children facing these prescribed drug cocktails are not receiving adequate care, reflecting a broader crisis within the mental health and pharmaceutical sectors that requires urgent action and change.
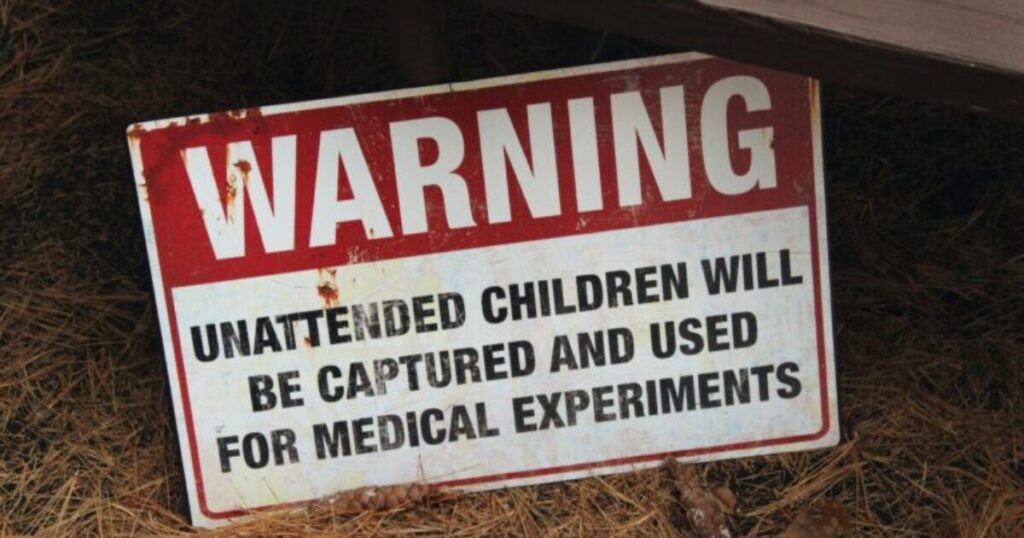
Ultimately, Hoft’s discourse sheds light on a critical narrative concerning the intersection of mental health treatment and the welfare of children. The increasing reliance on polypharmacy in pediatric care, compounded by a lack of scientific validation and oversight, signals an urgent need for reform. Advocating for transparency, informed consent, and more rigorous scientific investigation into psychiatric treatments can foster an environment where the mental health of children is not treated lightly or recklessly. Supporting organizations dedicated to child welfare could contribute to systemic change, ensuring that all children receive compassionate, evidence-based mental health care rather than merely being subjects of pharmaceutical experiments.