In a pioneering study, a 25-year-old woman with type 1 diabetes has become the first patient to achieve insulin independence following a transplant of reprogrammed stem cells derived from her own body. This remarkable case, reported in Nature and published in Cell Today, reveals a significant advancement in diabetes treatment, showcasing the potential of personalized stem cell therapies. The woman, who resides in Tianjing, China, began producing her own insulin just three months after undergoing the procedure, thus offering hope for a more effective management of, and possibly a cure for, type 1 diabetes.
The research, conducted by a team led by cell biologist Deng Hongkui at Peking University in Beijing, involved reprogramming cells taken from three individuals with type 1 diabetes back to a pluripotent state. This pluripotency allowed the researchers to produce various types of cells needed in the body, mimicking the essential insulin-producing islets typically lost in patients with diabetes. Notably, the scientists adapted an existing cellular reprogramming technique created by Shinya Yamanaka, replacing proteins with small molecules to enhance the process’s control and effectiveness.
To evaluate the safety and efficacy of this innovative treatment, the researchers generated three-dimensional clusters of insulin-producing islets from chemically induced pluripotent stem (iPS) cells and conducted trials in mice and non-human primates. The transformative surgery took place in June 2023 when approximately 1.5 million islets were injected into the woman’s abdominal muscles. This novel transplant site allowed for advanced monitoring through MRI scans, providing an opportunity for intervention if the cells did not function as intended.
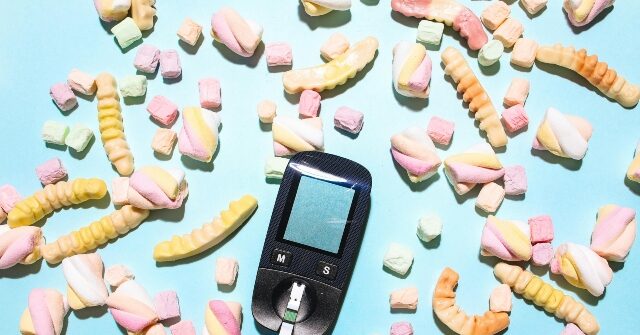
Remarkably, less than three months post-surgery, the patient was able to produce sufficient insulin independently, eliminating her need for daily insulin injections. For over a year, she has maintained stable blood glucose levels, reporting that they remain within the target range for more than 98% of the day. The woman expressed her altered quality of life, indicating newfound freedom in her diet, including the ability to consume sugar and other formerly restricted foods. This dramatic turnaround has garnered attention within the scientific community, with transplant surgeon James Shapiro noting the study’s groundbreaking achievement in reversing diabetes in a patient who previously required significant insulin supplementation.
While the initial results are highly promising, experts advise caution in proclaiming this treatment as a definitive "cure." They emphasize the necessity of replicating these outcomes in a larger cohort of patients over an extended period to thoroughly assess durability and safety. Furthermore, due to the patient’s prior liver transplant requiring immunosuppressant therapy, the current study could not directly measure whether the reprogrammed iPS cells would improve the risk for graft rejection.
In parallel, other research teams are also advancing the field of stem cell therapy for diabetes. Groups have initiated trials using insulin-producing islets derived from donor stem cells, which may offer a more scalable and commercially viable solution compared to the autologous approach seen in this groundbreaking case. Vertex Pharmaceuticals has reported preliminary positive results from a trial involving islets made from donated embryonic stem cells, with some participants achieving insulin independence within three months of their transplantation. These advancements reflect a growing momentum toward innovative treatments aimed at addressing diabetes, signifying a critical step forward in regenerative medicine and personalized healthcare.