The issue of COVID-19 vaccination and its impact on antibody levels, particularly mucosal IgA antibodies, is a significant topic within the scientific community. A pivotal study published on April 25, 2022, highlights the relationship between mRNA vaccination and the body’s immune response. Specifically, it was identified that effective interception of respiratory viruses hinges on the elevation of mucosal IgA antibodies, particularly those targeting the receptor binding domain (RBD) of the virus. The premise is straightforward: any successful vaccine should enhance these first line defenses, yet this study presents troubling findings—post-vaccination, individuals exhibited a marked decrease in mucosal IgA levels, leading to potentially increased susceptibility to the virus rather than the intended protective effect.
The ramifications of these findings are both alarming and critical to understanding the pervasive impact of COVID-19 vaccines on public health. The research indicated that, in many vaccinated individuals, levels of these antibodies fell to what were deemed ‘unmeasurable’ levels shortly after vaccination. This suggests a reversal of immune protection that individuals might have maintained prior to receiving the vaccine, which is a stark contrast to the expectations set forth prior to vaccine rollouts. Despite the enormity of these implications, the data produced remained primarily overlooked or unaddressed across notable segments of the medical community and mainstream media, ultimately obscuring an urgent public health message about the real effects of the vaccines.
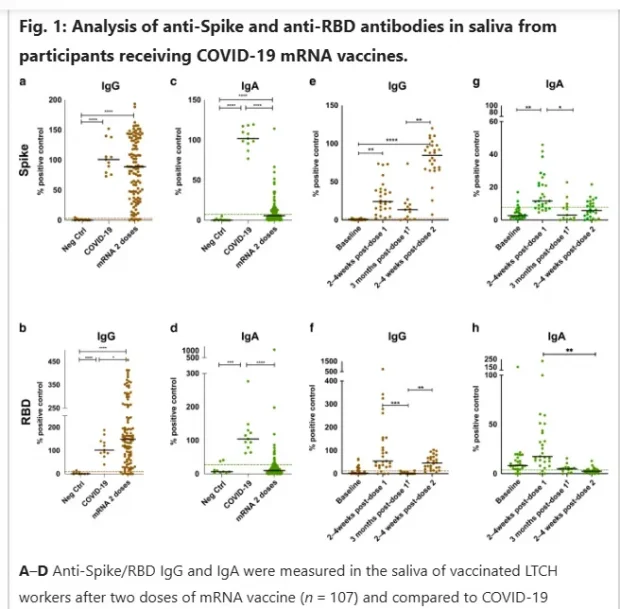
Figures presented in the study substantiate the findings, illustrating a dramatic decline in antibody levels from pre-vaccination states to post-vaccination measurements. The study featured a pivotal chart that displayed baseline RBD IgA levels compared to those taken two to four weeks after the second vaccine dose. The data unambiguously demonstrated that most subjects ended up with antibody levels significantly below previous measurements. Such a dramatic drop indicates that rather than bolstering the immune response, vaccines may compromise existing immunity, presenting an alarming narrative that contradicts public health messaging during the pandemic.
While the authors of the research do not explicitly cite the decline in RBD IgA levels as a failure of the vaccine, it is instrumental in understanding the reported efficacy of the vaccines. The initial claims of a 95% efficacy rate could not feasibly coexist with the observed depletion of critical immune components, which raises substantial concerns about the integrity of phase three trials that informed public endorsement of these vaccines. A thorough analysis calls into question the validity of conclusions drawn regarding the vaccines’ roles in curbing infection. Consequently, it can be argued that widespread messaging from public health authorities may have contained misinformation regarding the protective capabilities of the vaccines, misguiding public health policy and individual health choices.
Moreover, while the original study captured the essence of this pivotal immune response, more recent literature continues to build on this theme, albeit without adequately addressing the key findings regarding RBD IgA. The lack of emphasis on such critical components in later studies risks perpetuating a misunderstanding about the immune dynamics at play post-vaccination. Additionally, without embracing these findings, further studies may very well be set adrift in a narrative that continues to neglect foundational immune principles responsible for human health protection against respiratory viruses.
In conclusion, this analysis elucidates serious concerns about the COVID-19 vaccine’s actual impact on mucosal IgA immunity. The stark contrast between vaccines’ purported preventative capabilities and the measurable declines in critical immune response elements casts doubt on the overarching narrative of public health authorities. There has been a profound absence of critical engagement with this data within the scientific community and public discourse, leading to potential ramifications on health policy and pandemic management. As discussions around vaccine efficacy continue and further research emerges, it is necessary for the scientific community to confront these findings transparently, ensuring that public health narratives align with empirical evidence to guide informed citizen health decisions effectively.